Bone Health
Why does Bone Health matter in both younger and older people?
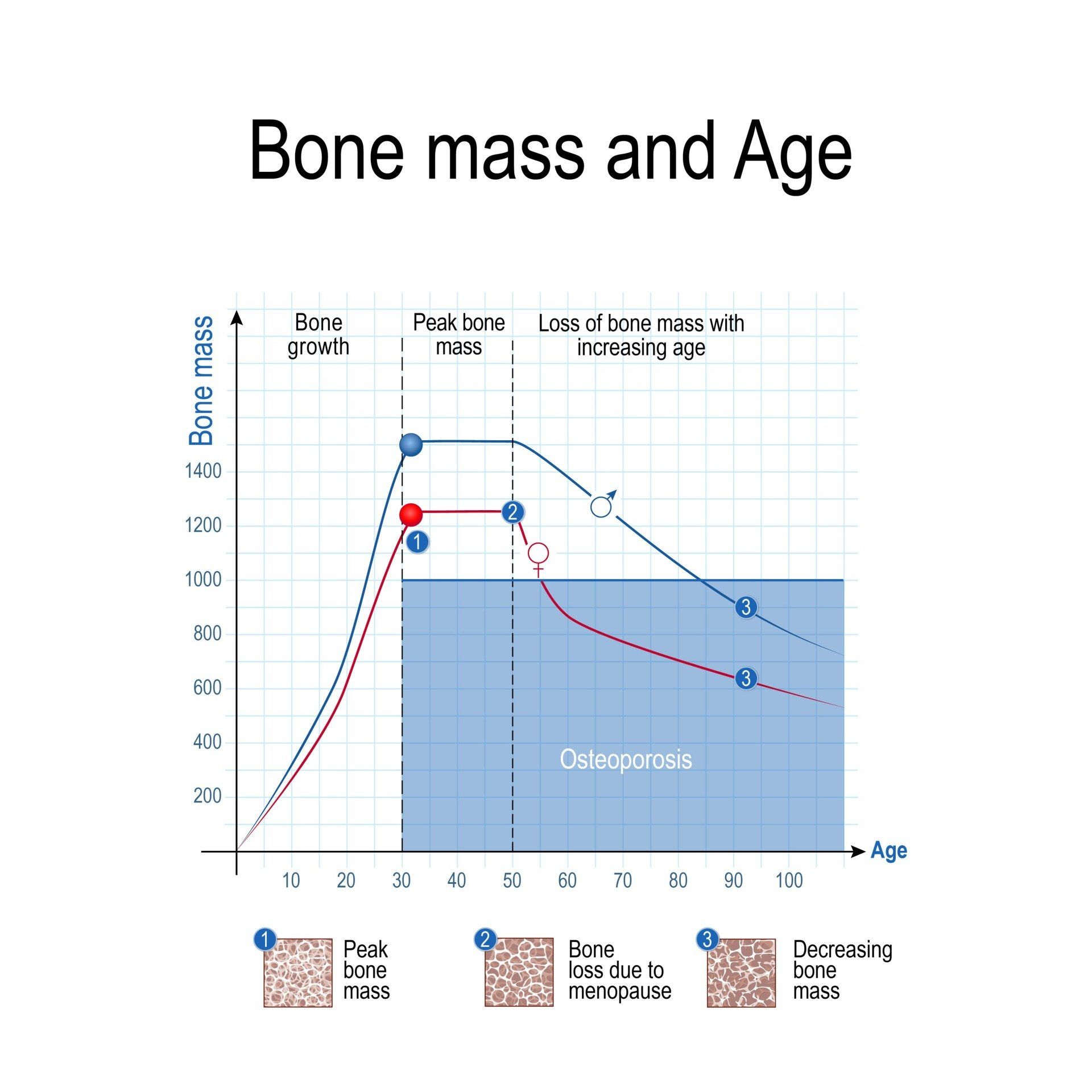
Our bone health is important because as we age, there is a natural decline in bone mineral density. This leads to an increased risk of fracture as bones become weaker.
Bone mass is a description of the proportion of the bodies weight that is made of bone tissue.
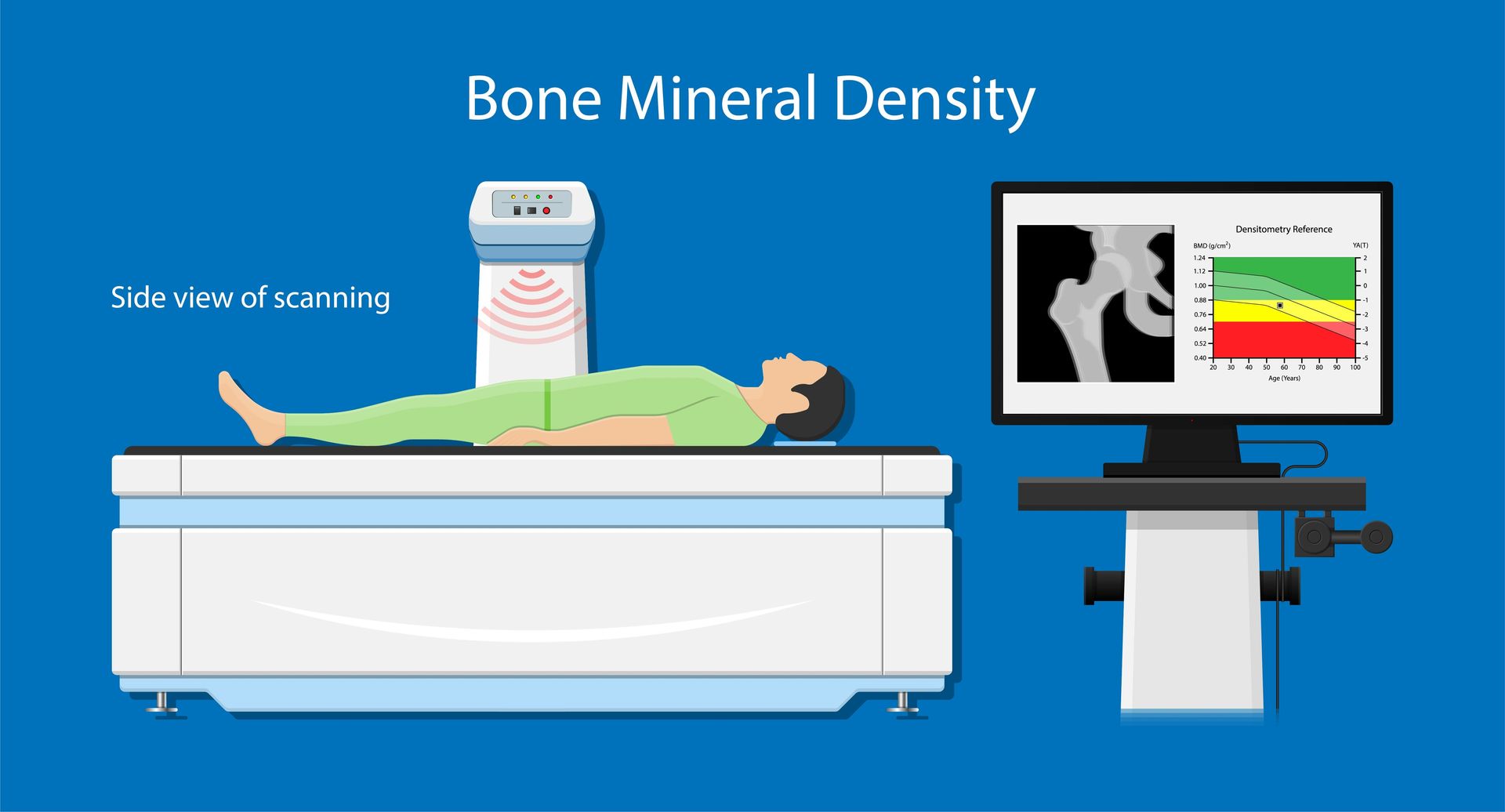
This can be measured using technology that passes very low dose x-rays through the body, since the denser, mineralised bone tissue stops the passage of x-rays more than other tissues. This is called DEXA or dual energy x-ray absorptiometry.
Bone architecture is the structure of the internal struts of bone, which also contribute to its strength. This can also provide important information because a person with low bone density is less likely to have a fracture if their bone struts are well formed to provide more structural integrity to their bones. This is measured using CT scans- but these deliver much higher radiation to the body.
While we often think of Osteoporosis and low bone mass as conditions of older people (and post-menopausal women in particular), the condition can and does start in young people, even if they are active . WE REACH OUR PEAK BONE DENSITY AT AGE 30 AND FROM THERE IT GOES DOWN
PREVENTION of low bone mass is much more effective than treatment because once there is significant loss of bone mass after the age of 30
The exception to this is the cessation of use of drugs such as the progesterone-only pill in women, which we know can lead to significant reversal of lost bone mass.
How can I find out if I have Low Bone Mass?
We offer
DEXA scanning
at Progressive Sports Medicine, as a part of our comprehensive service.
While anyone with clinical suspicion for low bone density may undertake a BMD test on a DEXA scan with clinical reasoning, testing may involve a Medicare rebate (with varying frequencies either every 12 months or every 24 months), for the following reasons:
- Broken bones or fractures in last ten years, caused by minimal trauma OR
- Monitoring proven low bone density (Osteoporosis) from previous DEXA or CT scan with a T score of -2.5 or less.
- Began menopause or had complete hysterectomy before the age of 45 years OR
- Currently taking Prednisolone or corticosteroid treatments and have done so for >4months OR
- Low testosterone in males
- Patients diagnosed with rheumatoid arthritis, chronic liver or kidney disease, hepatitis, Crohn’s,Coeliac, Graves, Hashimoto’s, malabsorptive disorders or an overactive thyroid.
- Have been diagnosed with osteoporosis (via DEXA or CT scan) and have had significant change of treatment (ie; started treatment or had a change in class of drugs, ie moved from Fosamax to Prolia ).
- Monitoring for those aged 70 or older and has a T- Score from previous BMD between -1.5 and -2.4.
- Patient is 70 years or older and not previously had a BMD examination ( initial scan ) ;
- Patient has a T- Score from a previous BMD of -1.5 and above.
What are the Causes of Low Bone Mass (Osteoporosis and Osteopenia)?
There are a number of factors that can lead to lower than expected bone mass, even in athletes. These include:
-Smoking, alcohol intake
-Low protein diets (especially if followed for many years)
-Relative energy deficiency and eating disorders (common in athletes in aesthetic sports like dance and gymnastics)
-Oral steroid use (glucocorticoids not anabolic steroids)
-Strong family history and genetic contributors
These factors are important in calculating a person's risk of a fracture as they age, and can be combined with the bone density score to give a good estimate.
As a general rule, if the 10 year risk of a major fracture is more than X%, the Y guidelines recommend that doctors consider pharmacological (drug) treatment for their patient.
What are the Treatment Options for Low Bone Mass (Osteopenia and Osteoporosis)?
There is a time and a place for medications to manage osteoporosis. These medications do prevent fractures but they do have some side effects and are not an adequate standalone therapy. The XX Guidelines recommend that physicians consider medication options if the calculated risk of fracture is . The modifiable risk factors such as smoking, are just important to remove if possible. The medications do nothing for reducing risk of falls and they do not restore bone architecture.
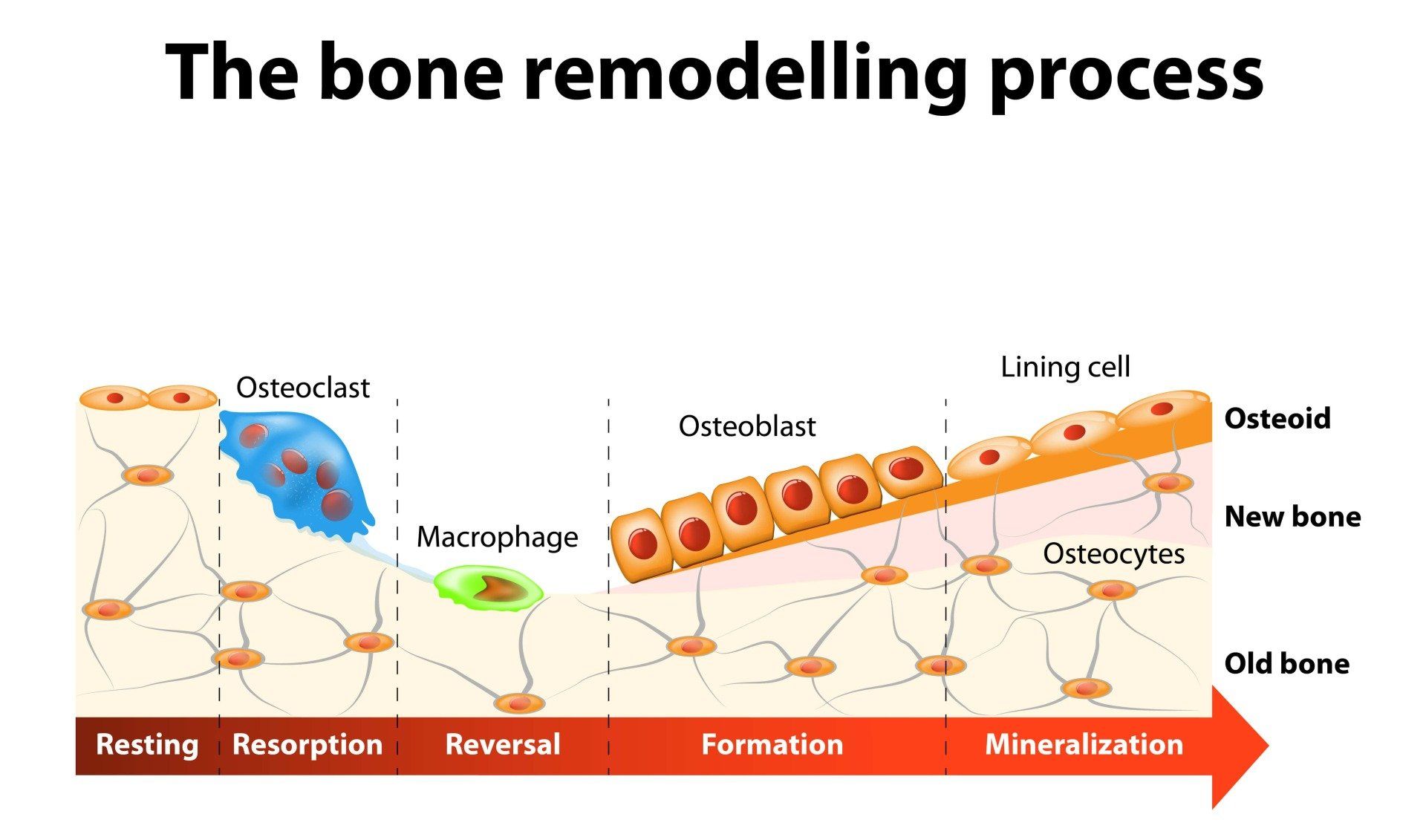
Most medications used for low bone mass do NOT build up new bone. They use various mechanisms to reduce resorption of bone. These medications include Bisphosphonates and Denosumab (Prolia). Some medications have been found to improve bone density on scans without reducing the risk of fracture significantly (Strontium). Pulsatile parathyroid hormone use is the only therapy that actually increases new bone formation by stimulating the cells that lay down new bone (Osteoblasts).
Since bone is a living tissue that senses how much load is being placed through it, and responds by making more or less of itself in response to that load, exercise is a critically important tool to maximise and bone health. Exercise costs nothing and has very few side effects.
The exercise that produces the most effect on bone are those that involve peak bone strain such as impact activities (e.g. hopping) and strength training. Lighter, low impact activities such as cycling and swimming do not reach the critical threshold to provide stimulus to bone formation. Lifting heavy enough weights, even with machines or cables, can provide adequate stimulus without the high joint forces from impact activity. The problem with impact activities in older patients is that they often exacerbate joint pain and bone bruising when there is wear and tear of cartilage.
Peak bone mass is achieved at about age 30. Before this stage, there is scope to significantly improve bone density because further bone accrues until about age 30. But once the skeleton is mature, there is a decline in bone mass at an average of 1% per year (and over 2-3% per year post-menopause) and it is much more difficult to gain bone mass. The emphasis then shifts to maintaining bone mass and preventing rapid decline.
A more controversial area of medicine is the use of Hormone Replacement Therapy for the treatment of menopausal symptoms and low bone mass. There is good evidence that estrogen helps preserve bone mineral density, and following menopause there is a precipitous decline in estrogen levels that leads to a more rapid decline in bone mass.
However, the risks and benefits of such treatment need to be weighed up between patient and physician in each individual case.





