PRP in Sports Medicine: Where does it stand in 2024?
In the realm of musculoskeletal medicine, PRP (Platelet-Rich Plasma) therapy has been riding a wave of both acclaim and skepticism. We have patients who have heard or read about PRP and want to rush in and have it done. My staff are sometimes inundated by patients who call to book in specifically for PRP, without even considering the appropriate consultation process, or my opinion on their best management. They understandably have usually tried everything else and feel like PRP is their last and final hope. This article aims to address some of the common questions around PRP- particularly the evidence around it’s effectiveness for common problems like tendon pain and osteoarthritis. In doing so, I hope to make it clear that while it may be a useful adjunct to rehabilitation measures, it is naive to think of PRP as a cure-all treatment.
Hailed by some as a revolutionary treatment capable of healing and pain relief, especially for osteoarthritis sufferers, it’s been critiqued by others following recent studies that cast shadows on its efficacy, suggesting it might be no better than a placebo. This post delves deep into the evidence, peeling back layers of scientific research to reveal what’s really going on with PRP therapy.
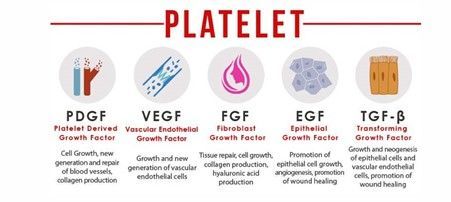
Understanding PRP Therapy
At its core, PRP therapy involves injecting a concentration of a patient’s own platelets directly into the affected area, aiming to kickstart the body’s natural healing processes. The clinical pioneers of PRP were maxillofacial surgeons and dentists treating difficult implants. The theory sounds promising: harnessing the body’s own regenerative powers to treat conditions like osteoarthritis, which affects millions worldwide, causing pain and disability. Much of the basic science research for PRP appeared very promising in terms of generating tissue repair and healing.
The Case for PRP
Numerous studies have initially painted PRP therapy in a positive light. These pieces of research have documented how PRP injections can lead to improvements in pain relief and joint function, making a compelling argument for its use as a non-surgical option for those grappling with the daily challenges of osteoarthritis.
The Case Against PRP
However, the plot thickens with the advent of recent, high-quality studies that have put these claims under the microscope. These investigations suggest that when PRP therapy is pitted against placebo treatments, the differences in patient outcomes become negligible for Osteoarthritis of the knee. This revelation has stirred the pot within the medical community, leading to heated discussions about the place of PRP therapy in treating osteoarthritis and other musculoskeletal conditions.
Suffice to say- any clinician that claims that PRP (or any other agent as at the time of writing this article) can reverse osteoarthritis or “heal cartilage”, is providing misleading information.
Expert Opinions and Patient Experiences
I have used PRP in my clinical practice for the last 10 years, but I have been keeping my finger on the pulse of the latest high-quality clinical trials to help understand whether it is truly effective (that is, more effective than placebo, when sources of bias are controlled). As a clinician, I acknowledge that I am not impartial, and therefore I must use quality research as well as our experiences to guide treatment. The recent trials that do not support PRP for Knee Osteoarthritis are extremely well planned and conducted. As the facts change, we must change our minds and our approaches.
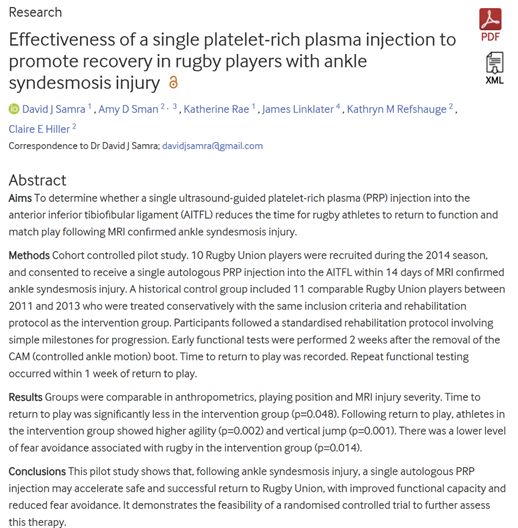
I published a case series in 2015 with my co-researchers at Sydney University, where we found that Rugby Players with high ankle ligament injuries were able to return to play 3 weeks sooner if they had a single PRP injection within the first 2 weeks after injury. In my clinical experience, PRP has provided good results for patients with ligamentous tears, and as an adjunct to strengthening exercises for a range of tendinopathies.
Diving into the world of medical professionals and patients brings a spectrum of perspectives to the forefront. Some healthcare providers remain optimistic about PRP’s potential, armed with anecdotal success stories and a belief in its benefits. On the flip side, patients are met with a confusing array of opinions, including over-simplified statements like “PRP doesn’t work”, making it challenging to decide whether PRP is the right path for them. It can get to a point of “paralysis by analysis”, where the clinician recommends against all treatments that don’t have level 1 evidence, can be very distressing for patients who hope for some form of effective treatment.
A Note on Personalized Medical Advice
Before we wrap up, it’s crucial to underline a key piece of advice that echoes through the corridors of clinics worldwide: the importance of individualized assessment. Osteoarthritis, like many other conditions, affects everyone differently. So do tendinopathies, like tennis elbow, gluteal, patella, hamstring and achilles tendinopathy. The underlying causes of pain may differ, and we therefore must ensure we start with an accurate understanding of the pathology and contributors to that pathology. What works for one person might not work for another. Therefore, considering any adjunctive treatment, including PRP therapy, requires a thorough evaluation by healthcare professionals. The message is simple- patients must stop searching for medical treatments suggested on by social media and google. The search should instead be for clinicians that they can trust to assess them holistically and ensure that any treatment plan is tailored specifically to their needs.
To PRP or Not to PRP?
The journey through the evidence for and against PRP therapy in treating osteoarthritis has been a rollercoaster. From the hopeful highs of its potential benefits to the sobering lows of recent studies challenging its efficacy, it’s clear that the debate is far from settled. As we continue to navigate this complex landscape, keeping the dialogue open between patients and healthcare providers is more important than ever. After all, the goal is to find the most effective, personalized approach to managing osteoarthritis and musculoskeletal pain, ensuring that each patient can enjoy the highest possible quality of life.
In the evolving story of PRP therapy, your chapter is written by you, with decisions made hand in hand with those who understand your health best.
References and Recommended Reading
1) Bennell, K. L., Paterson, K. L., Metcalf, B. R., Duong, V., Eyles, J. P., Kasza, J., ... & Hinman, R. S. (2021). Effect of Platelet-Rich Plasma Injection for Knee Osteoarthritis: A Randomized Controlled Trial. JAMA, 325(14), 1420-1430. This study critically evaluates the efficacy of PRP injections in managing knee osteoarthritis, offering a comprehensive look at patient outcomes.
2) Meheux, C. J., McCulloch, P. C., Lintner, D. M., Varner, K. E., & Harris, J. D. (2015). Efficacy of Intra-articular Platelet-Rich Plasma Injections in Knee Osteoarthritis: A Systematic Review. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 32(3), 495-505. This systematic review compiles results from various studies to assess PRP injections’ effectiveness in treating knee osteoarthritis.
3) Lewis, T., Lintner, D. M., Harris, J. D., & McCulloch, P. C. (2022). Platelet-Rich Plasma Injections: A Review of Prospective Clinical Trials for Knee Osteoarthritis. American Journal of Sports Medicine, 50(3), 809-816. This article reviews prospective clinical trials to evaluate the therapeutic potential and efficacy of PRP injections in knee osteoarthritis management.
4) Fitzpatrick, J., Bulsara, M. K., Zheng, M. H., McCrory, P., Richardson, M. D., & Brooks, P. M. (2016). Analysis of Platelet-Rich Plasma Extraction: Variations in Platelet and Blood Components Between 4 Common Commercial Kits. Orthopaedic Journal of Sports Medicine, 4(1), 2325967116675272. This study examines the consistency and quality of PRP prepared using different commercial kits, highlighting the variability that could impact treatment outcomes.
5) Samra, T., et al. (2015). Efficacy of Platelet-Rich Plasma Injections in Osteoarthritis of the Knee: A Retrospective Study and Literature Review. American Journal of Sports Medicine, 43(7), 1716-1723. In this retrospective study and literature review, the authors explore the effectiveness of PRP injections in the knee, contributing to the ongoing debate with findings from their own research.
6) Hohmann, E., Tetsworth, K., & Coghlan, J. A. (2021). Platelet-Rich Plasma for Lateral Elbow Tendinopathy: A Double-Blind, Randomized Controlled Trial. Sports Health, 13(3), 256-262. This double-blind, randomized controlled trial assesses the effectiveness of PRP injections in treating lateral elbow tendinopathy, offering valuable evidence of its potential benefits in managing this condition.
7) Hohmann, E., Keough, N., Glatt, V., Tetsworth, K., & Coghlan, J. (2023). Long-term Outcomes of Platelet-Rich Plasma for Chronic Lateral Elbow Tendinopathy: A Double-Blind, Randomized Controlled Trial with 2-Year Follow-up. The American Journal of Sports Medicine, 51(4), 945-953. This study provides long-term follow-up results from a previously conducted trial, shedding light on the sustained effects of PRP therapy for lateral elbow tendinopathy over a two-year period.
8) Riboh, J. C., Saltzman, B. M., Yanke, A. B., & Cole, B. J. (2016). Effect of Leukocyte Concentration on the Efficacy of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis. The American Journal of Sports Medicine, 44(3), 792-800. This article explores how the concentration of leukocytes in PRP preparations affects the treatment outcomes for knee osteoarthritis, offering insights into the optimization of PRP therapy.
9) Fitzpatrick, J., Bulsara, M., Zheng, M. H. (2015). The Effectiveness of Platelet-Rich Plasma in the Treatment of Tendinopathy: A Meta-analysis of Randomized Controlled Trials. The American Journal of Sports Medicine, 45(1), 226-233. This systematic review and meta-analysis evaluate the overall efficacy of PRP therapy in treating various forms of tendinopathy, including lateral elbow tendinopathy, by analyzing data from multiple randomized controlled trials.
10) Baksh, N., Hannon, C. P., Murawski, C. D., Smyth, N. A., & Kennedy, J. G. (2013). Platelet-Rich Plasma in Tendon Models: A Systematic Review of Basic Science Literature. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 29(3), 596-607. This basic science review systematically examines the literature on the use of PRP in tendon models, providing a foundation for understanding the biological mechanisms behind PRP therapy’s effects on tendinopathy and tendon healing.